Understanding plantar fasciitis and how to ease it is vital for anyone who experiences recurring heel pain. This condition affects thousands of people each year, often making it difficult to walk, exercise, or stand for long periods.
While some treatments are straightforward, long-term relief requires a combination of lifestyle adjustments and supportive care.
Even simple tools like learning how do corn removal pads work can highlight the importance of pressure relief in foot health. This article explains what plantar fasciitis is, why it happens, and practical ways to manage it.
What Is Plantar Fasciitis?
Definition
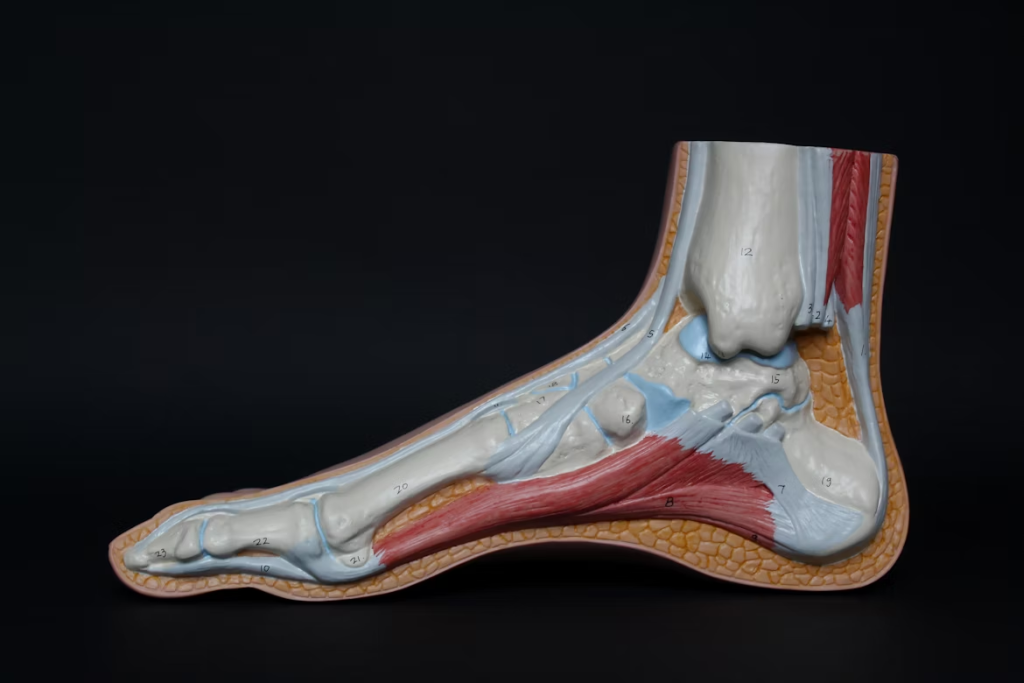
Plantar fasciitis is an inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of the foot, connecting the heel bone to the toes. When strained, the fascia develops small tears that lead to pain and stiffness.
Key Symptoms
- Sharp heel pain when taking the first steps in the morning.
- Discomfort after long periods of standing or sitting.
- Pain that worsens after exercise rather than during.
Who It Affects
Plantar fasciitis is common among runners, teachers, retail workers, and anyone who spends long hours on their feet. It also affects people with flat feet, high arches, or tight calf muscles.
Understanding Plantar Fasciitis and How to Ease It Through Risk Awareness
Foot Mechanics
Flat feet, high arches, or abnormal walking patterns can increase strain on the fascia, leading to irritation over time.
Footwear Choices
Shoes with little cushioning or poor arch support contribute to the problem. Wearing thongs, high heels, or worn-out trainers increases the risk.
Activity Levels
Sudden increases in exercise, especially running or jumping activities, place stress on the heel. Repetitive strain without proper recovery makes inflammation worse.
Weight and Pressure
Excess body weight adds extra load to the feet, making it harder for the fascia to recover from daily pressure.
Early Warning Signs
Morning Pain
A sharp or stabbing sensation in the heel during the first few steps of the day is one of the clearest indicators.
Swelling and Tenderness
Some people notice localised swelling or a tender spot under the heel.
Stiffness
Stiffness in the heel or arch after long periods of sitting suggests inflammation is present.
Understanding Plantar Fasciitis and How to Ease It with Home Remedies
Rest and Recovery
Giving the fascia time to heal is the first step. Avoid activities that cause repeated stress, such as long runs or jumping.
Ice Therapy
Applying ice for 15–20 minutes reduces swelling and numbs the pain. Rolling the heel over a frozen water bottle provides targeted relief.
Stretching Exercises
Gentle stretches for the calves and plantar fascia reduce tension. A common method is pulling the toes back toward the shin to lengthen the tissue.
Supportive Footwear
Wearing shoes with good cushioning and firm arch support prevents strain. At home, supportive sandals are better than walking barefoot on hard floors.
Strengthening the Foot
Calf Raises
Standing on the edge of a step and raising the heels strengthens calf muscles, reducing tension on the fascia.
Towel Scrunches
Placing a towel on the floor and pulling it toward you with your toes strengthens small foot muscles.
Ball Rolling
Rolling the arch over a tennis or massage ball loosens tight tissue and stimulates circulation.
Strengthening exercises are simple, yet they support long-term improvement.
Professional Treatments
Podiatry Support
Podiatrists provide tailored advice, recommend orthotics, and offer specific stretching programmes. They may also use taping methods to offload pressure from the fascia.
Physical Therapy
Therapists guide patients through progressive strengthening and flexibility exercises. They may use ultrasound or manual therapy to reduce pain.
Injections
Steroid injections provide temporary relief in severe cases, though they are not a long-term solution.
Shockwave Therapy
This non-invasive treatment uses sound waves to stimulate healing in chronic plantar fasciitis cases.
Surgery
Surgical intervention is rare and usually only suggested when all other options fail. It involves releasing part of the fascia to reduce tension.
Orthotics and Support Devices
Custom Orthotics
Tailored inserts provide support by correcting abnormal walking patterns and distributing pressure more evenly.
Over-the-Counter Insoles
Prefabricated insoles can also help, particularly for those with mild cases.
Night Splints
Wearing a splint at night keeps the fascia stretched, preventing morning stiffness.
Compression Socks
Compression gear reduces swelling and provides support throughout the day.
Daily Habits That Support Recovery
Regular Stretching
Making stretching part of the daily routine helps keep tissues flexible. Morning and evening stretches prevent recurring stiffness.
Weight Management
Reducing body weight lowers the strain placed on the fascia, easing recovery and reducing recurrence.
Gradual Exercise Routines
Building up activity slowly rather than rushing into long runs or high-intensity workouts helps prevent setbacks.
Alternating Activities
Switching between high-impact and low-impact activities, such as cycling or swimming, reduces repeated stress on the fascia.
Preventing Plantar Fasciitis from Returning
Shoe Rotation
Rotating between pairs of shoes ensures they remain supportive for longer, as cushioning compresses over time.
Workplace Adjustments
Using anti-fatigue mats or sitting breaks can protect feet if you work long hours standing.
Regular Check-Ups
People prone to recurring pain benefit from periodic check-ins with podiatrists or physiotherapists.
Ongoing Strengthening
Maintaining strong and flexible muscles supports the fascia even after symptoms disappear.
Myths About Plantar Fasciitis
Myth 1: Only Runners Get It
While running increases risk, anyone who spends long hours standing or walking on hard surfaces can develop plantar fasciitis.
Myth 2: Pain Will Always Go Away with Rest
Rest helps, but without stretching, footwear adjustments, and strengthening, the condition often returns.
Myth 3: Surgery Is the Only Permanent Fix
Most people recover with conservative treatments. Surgery is a last resort for very severe, unresponsive cases.
Understanding Plantar Fasciitis and How to Ease It Through Lifestyle Changes
Nutrition and Healing
A balanced diet with adequate protein, vitamins, and minerals supports tissue repair.
Hydration
Staying hydrated keeps muscles and tissues supple, reducing stiffness.
Sleep and Recovery
Quality sleep allows the body to repair damaged tissue more effectively.
Lifestyle choices contribute significantly to both healing and prevention.
Conclusion
Understanding plantar fasciitis and how to ease it helps reduce pain, speed recovery, and prevent future flare-ups. Simple changes like supportive footwear, stretching, and daily strengthening can make a significant difference.
For stubborn cases, professional treatments and orthotics provide additional relief. By combining home care, lifestyle adjustments, and preventive habits, it is possible to manage plantar fasciitis effectively and return to comfortable, pain-free movement.
Frequently Asked Questions
How long does it take for plantar fasciitis to heal?
Most cases improve within 6–12 weeks with consistent home care. Chronic or severe cases may take several months, especially if treatment is delayed.
Can plantar fasciitis heal on its own?
Yes, some mild cases improve with rest and basic care. However, ignoring ongoing pain increases the chance of it becoming chronic.
What type of shoes are best for plantar fasciitis?
Shoes with cushioned midsoles, firm heel counters, and strong arch support are best. Avoid flat, unsupportive shoes such as thongs or thin-soled flats.
